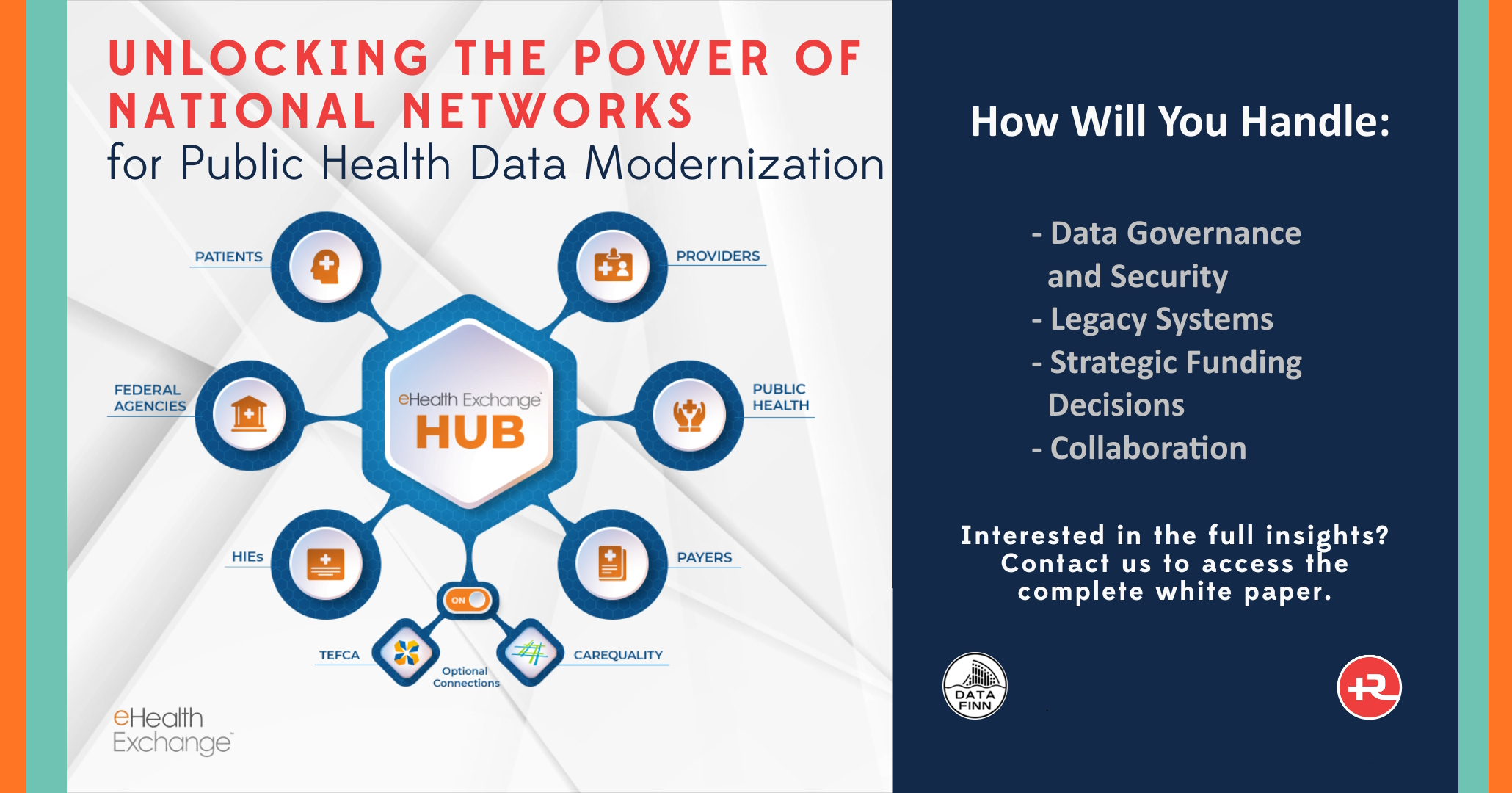
Unlocking the Power of National Networks for Public Health Data Modernization
Imagine trying to fight a wildfire while your team is scattered across the terrain, using walkie-talkies operating on different frequencies. I don’t have to tell you that public health data exchange often feels like that today. Data systems don’t easily talk to each other, responses are slow or missing, data is distorted by static, and tools are all too often outdated and inefficient.
But the good news is that we don’t have to start from scratch to modernize and improve on this picture. We have national networks such as APHL’s AIMS Platform and eHealth Exchange, that are ready and poised to help. These are two of the biggest existing highways of health data, securely processing billions of transactions a year. They are professional grade infrastructure that have already been built, are reliable, secure, and have modernized features ready to use.
With so many systems to deal with and potential new functionality at your disposal, where do you begin? Which datasets and systems should be connected first? Welcome to my world! After working through this process with a number of states, in consultation with Jeff Couch, Managing Partner of Ruvos, I have compiled a comprehensive public health data modernization framework that will soon be published. This white paper and toolkit is designed to help you determine the best way forward for your jurisdiction whether you’re just getting started, or already deep in the weeds. Drop me a line at contact@datafinn.com, and we’ll let you know as soon as it becomes available.
With that in mind, I’ll devote the remainder of this blog to outlining the advantages and considerations of joining national networks and how they help us to continue closing these gaps.
The Case for National Networks
Public health systems have long struggled with fragmented data and delays. Local systems don’t always share information easily, and critical insights can get lost in the shuffle. That’s where national networks can provide supplemental functionality around sharing the data you need between other agencies, or by offering a blueprint for robust, secure cloud architecture you can model as you modernize the local systems in your domain. These networks save time, reduce errors, and enable better decision-making which are all critical improvements in the public health domain.
The AIMS Platform is a proven tool for sharing lab data in real time which is essential when facing emerging health threats. The platform supports an ever-growing catalog of use cases, from Electronic Case Reporting, to Electronic Test Orders and Results. And it extends well beyond laboratory matters to host third-party services used by public health agencies nationally, such as STEVE – State and Territorial Exchange of Vital Events.
eHealth Exchange is a “network of networks” that links healthcare providers, government agencies, and non-profits, allowing them to share medical data for treatment purposes. They have been a leader in the movement to improve care coordination and healthcare interoperability for over a decade.
While it is true that these national networks have had some adoption issues over the years, progress when dealing with ecosystems as complex as healthcare takes time. Enter the Trusted Exchange Framework and Common Agreement (TEFCA). TEFCA provides overarching guidance that ties together existing national networks under one plan, making sure each type of data fits into a larger, coherent system. In addition to shared technical standards it also provides a robust legal infrastructure to clarify data use and removes barriers around data privacy and security. Most importantly, TEFCA is the first nationally endorsed exchange framework to include the voice of both patients and public health.
The Challenges of Leveraging National Health Networks
Leveraging national health networks must be done right to move the needle forward. Here are a few of the hurdles you will face that demand strategic thinking and collaboration.
Data governance and security are paramount. Agencies must adhere to strict privacy regulations. For modernization, this means cataloging and researching data-sharing agreements across systems and program areas so they can be uniformly aligned with regulations like TEFCA. It is important to establish a legal infrastructure and governance structures that are as robust as the networks themselves.
Legacy systems are the norm. Most public health systems are built on outdated infrastructure that wasn’t designed to integrate with modern networks. To bridge this gap, agencies need to reimagine who and how datasets are worked across public health while investing in shared technologies like scalable APIs, data enrichment, and data pipelines.
Strategic funding decisions are critical. With tight budgets, every dollar has to count toward meaningful modernization that aligns with public health goals. The focus isn’t just on upgrading but on maximizing impact across the public health enterprise.
Collaboration is the glue. Public health depends on teamwork—federal, state, and local agencies working together with aligned goals and clear communication. When everyone pulls in the same direction, real transformation happens.
Closing Thoughts
The road to public health data modernization is complex, but leveraging national networks like the AIMS Platform and eHealth Exchange can help simplify the journey. When combined with well-executed plans, these networks help unlock transformative change. Finding an experienced technical partner that understands the business of health data will simplify and accelerate your progress. You are not alone on your journey to improving public health! We’d love the opportunity to discuss your projects and see how we can help meet and exceed your data modernization goals.